Changes to Claims/Payment Process for Behavioral Health Providers- effective November 1, 2023
 Download PDF
Download PDF
The purpose of this bulletin is to inform Behavioral Health providers of actions they must take in order to continue to receive payments without interruption after November 1, 2023. Behavioral Health refers to both mental health (MH) and Addiction and Recovery Treatment Services (ARTS) providers.
Providers must take action as soon as possible in order to smoothly transition claims submissions to prevent interruption of payment for the November 1, 2023 go-live of the Service Authorization (SA) and Specialty Services contract.
As part of the transition project, Gainwell will be adding a VA FFS contract for the providers that currently have a PAR Magellan BHSA contract. These providers do not need to re-enroll.
Behavioral Health Providers – take action now!
1. If you do not currently have secure access to the MES PRSS Portal, please complete the Primary Account Holder (PAH) form and fax it to 888-335-8476.
a. Download the Primary Account Holder (PAH) form from the MES Public Portal. You can Download it here. The turnaround time to process PAH forms is generally 7-10 business days therefore it is imperative that providers act now so that your payment is not delayed.
b. If you already have a PAH, please reach out to the primary account holder (PAH) of your organization for the MES Provider Portal access. If you did not receive provider portal credentials and you are the designated primary account holder (PAH) for your organization, please submit a PAH update form using the new PRSS PAH update form available on the MES provider page at the following link: https://vamedicaid.dmas.virginia.gov/provider. If you have already sent this form and have additional questions about the form or your portal account access, please contact the PRSS help desk at 888-829-5373.
c. If you have a PAH with credentials and do not need any assistance, go to step 2.
2. Billing Providers must have the correct Electronic Funds Transfer (EFT) information in PRSS in order to receive payment to the provider’s correct banking facility. Follow the below steps for adding and/or updating EFT information to your provider file.
a. If you do not have EFT information on file, or needs to be updated, the required EFT Form is here.
b. Check you EFT information to assure it is correct.
c. Providers who have access to the MES PRSS Portal and have not set up EFT in PRSS must log on the secure provider portal and follow the instructions for adding EFT information, located on the MES Public Portal under provider training. Click on PRSS-120 “Provider Portal Overview” and download the training PDF (EFT instructions on page 60) or view the PRSS-120 “Provider Portal Overview” video.
d. instructions on how to access provider documents are in MES provider training PRSS- 120 “Provider Portal Overview” and are on page 121 or view the PRSS-120 Provider Portal Overview video. All providers enrolled with DMAS must also receive electronic remittance advices (ERA). Providers will have access to their remittance advices on the Secure MES Portal.
3. Billing providers who choose to act as their own clearinghouse and can create EDI X12 format files must set up as a Service Center in order to transmit and receive Electronic Data Interchange (EDI) X12 transactions, which includes submitting electronic claims and receiving remittances. Service Center is a term that DMAS uses for the entities that either send or receive EDI Transactions on behalf of a provider. This is also synonymously used as Trading Partner.
- Billing Providers and/or Clearinghouses Enrolling as a DMAS Service center
To exchange X12 EDI transactions directly with DMAS, the requester should contact DMAS via email: MESEDISupport@dmas.virginia.gov. A DMAS associate will review the request and enroll the billing provider as a service center. A 4-digit service center ID will be generated after the EDI enrollment.
- Review EDI related documents placed in the below link before proceeding https://vamedicaid.dmas.virginia.gov/edi#gsc.tab=0
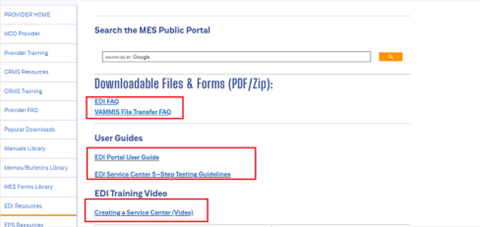
- Billing Providers who cannot create the EDI X12 format files must reach out to any of the following DMAS approved service centers and associate with them for submitting claims and receiving Remittance Advice’s (RA). For contact information on the Service Centers, review these FAQs at https://vamedicaid.dmas.virginia.gov/edi#gsc.tab=0.
Please ensure the service center is setup for the transaction type you need, i.e., 837I, 837P, 835/277U.
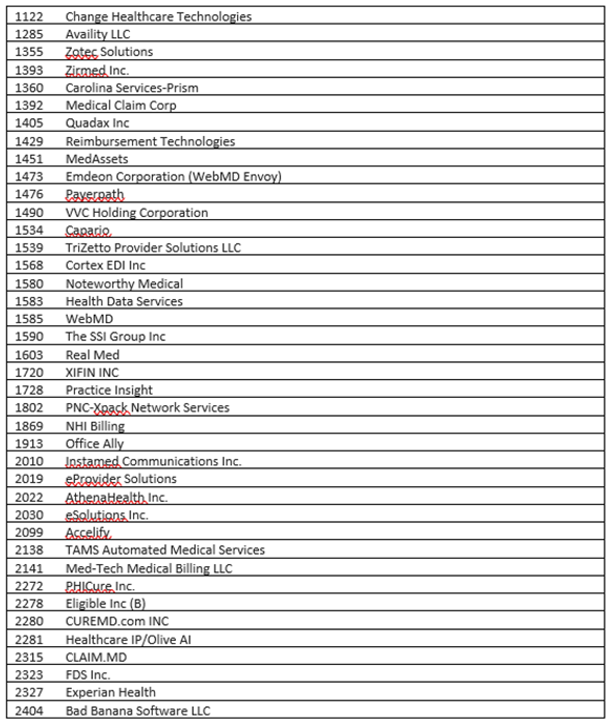
- DMAS Approved Service Centers List:
- Providers associating with a service center:
When a Provider wants to exchange transactions using a clearinghouse/Service center, the provider must associate their NPI with the clearinghouse/service center for those transaction types in order to submit claims or receive RA’s. Review EDI Training video for association steps. Managing Service Center Authorizations (Video)
- If you are an existing Provider or an existing Provider already associated with a service center, have a valid 4-digit service center ID and are currently submitting the same type of claims (837 Institutional or Professional) to DMAS (not through Magellan BHSA) and receiving remittances from DMAS – No action is required.
Note: A 4-digit service center ID is required in order to exchange data electronically with DMAS for November 1, 2023.
- Direct Data Entry (DDE) Providers may submit Professional (CMS-1500), Institutional (UB-04) and Medicare Crossover claims using Direct Data Entry (DDE). Providers also may make adjustments or void previously submitted claims through DDE. DDE is provided at no cost to providers. Paper claims submissions are not allowed except when requested by DMAS. Providers must use the Medicaid Enterprise System (MES) Provider Portal to complete DDE
Access to Claims Direct Data Entry (DDE) is via the MES Provider Portal (Login Required):
PRSS portal. https://login.vamedicaid.dmas.virginia.gov/SecureISS/landingpage
Users will need to be associated with a billing provider and must be the Primary Account Holder (PAH) or assigned credentials by a PAH or Delegated Admin (DA).
Previous Bulletin and Magellan memo blast that went out to providers, requested the following:
- They update and/or add their EFT information if they are a biller.
- To complete the Primary Account Holder (PAH) form if they have not already done so.
- To submit their Service Auth’s to Kepro/Acentra Health starting November 1, 2023.
- To submit their claims to Conduent, DMAS’s fiscal agent.
- Previous bulletin that went out with this information can be found here: https://vamedicaid.dmas.virginia.gov/bulletin/bhsa-changes-due-magellan-contract-ending-electronic-funds-transfer-update-required
For more information, please visit the MES Provider Training page. This page includes a curriculum and comprehensive list of provider courses.
Virginia Medicaid Web Portal Automated Response System (ARS) Member eligibility, claims status, payment status, service limits, service authorization status, and remittance advice. | |
Medicall (Audio Response System) Member eligibility, claims status, payment status, service limits, service authorization status, and remittance advice. | 1-800-884-9730 or 1-800-772-9996 |
Acentra Health Service authorization information for fee-for-service members.
| |
Provider Appeals DMAS launched an appeals portal in 2021. You can use this portal to file appeals and track the status of your appeals. Visit the website listed for appeal resources and to register for the portal. | |
Managed Care Programs Medallion 4.0, Commonwealth Coordinated Care Plus (CCC Plus), and Program of All-Inclusive Care for the Elderly (PACE). In order to be reimbursed for services provided to a managed care enrolled individual, providers must follow their respective contract with the managed care plan/PACE provider. The managed care plan may utilize different guidelines than those described for Medicaid fee-for-service individuals. | |
Medallion 4.0 | |
CCC Plus | |
PACE | |
Magellan Behavioral Health Behavioral Health Services Administrator, check eligibility, claim status, service limits, and service authorizations for fee-for-service members. | www.MagellanHealth.com/Provider www.magellanofvirginia.com, email: VAProviderQuestions@MagellanHealth.com,or Call: 1-800-424-4046 |
Provider Enrollment | In-State: 804-270-5105 Out of State Toll Free: 888-829-5373 Email: VAMedicaidProviderEnrollment@gainwelltechnologies.com |
Provider HELPLINE Monday–Friday 8:00 a.m.-5:00 p.m. For provider use only, have Medicaid Provider ID Number available. | 1-804-786-6273 1-800-552-8627 |
Aetna Better Health of Virginia | www.aetnabetterhealth.com/Virginia 1-855-270-2365 1-866-386-7882 (CCC+) |
Anthem HealthKeepers Plus | 1-833-207-3120 1-833-235-2027 (CCC+) |
Molina Complete Care
| 1-800-424-4524 (CCC+) 1-800-424-4518 (M4) |
Optima Family Care | 1-800-643-2273 1-844-374-9159 (CCC+) |
United Healthcare | 1-844-284-0149 1-855-873-3493 (CCC+) |
Dental Provider DentaQuest | 1-888-912-3456 |
