Change In Enrollment Policy for Certain Dual Eligible Medicare-Medicaid Enrollees
 Download PDF
Download PDF
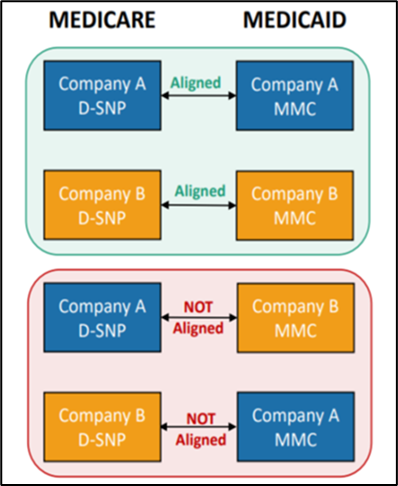
The purpose of this bulletin is to inform providers that beginning January 1, 2025, full benefit dual eligible Medicaid enrollees that have elected to enroll in a type of Medicare Advantage (MA) Plan called a Dual Eligible Special Needs Plan (DSNP) will be assigned to the same health plan for their Medicaid managed care as they selected for their DSNP. This alignment of Medicare and Medicaid health plan enrollment is generally referred to as “exclusively aligned enrollment.”
Who is impacted
Dual eligible enrollees (duals) are persons who are eligible for and enrolled in both Medicare and Medicaid. There are two types of dual eligible enrollees: (1) Full Benefit Duals, who are persons that receive full Medicare and full Medicaid, and (2) Partial Benefit Duals, who are persons that receive full Medicare but whose income exceeds Medicaid eligibility requirements but is low enough that the State pays their Medicare coinsurance and/or deductible.
For their Medicare coverage, dual eligible enrollees can choose to enroll in Medicare Fee-For-Service (sometimes called original Medicare) and a Part-D (prescription coverage) plan, or they can enroll in a MA plan (sometimes call Medicare Managed Care or Part-C Plan), including a DSNP. For their Medicaid coverage, with a few exceptions, full benefit duals must enroll with one of Virginia’s five managed care plans. Partial benefit duals are excluded from Medicaid managed care.
Staring January 1, 2025, full benefit dual eligible enrollees who are in Medicaid managed care and have elected to enroll in a DSNP will have their health plan enrollment aligned. Full benefit dual eligibles who are excluded from Medicaid managed care (such as those who reside in an excluded facility), are enrolled in Medicare Fee-For-Service or a non-DSNP MA plan, and partial benefit duals will not be impacted.
Why this change is happening
DSNPs are a type of MA plan that must contract with the Department and that can only enroll dual eligible enrollees and are specifically designed to meet the unique needs of duals. DSNPs must integrate or coordinate Medicare and Medicaid benefits. Each state determines the level of integration or coordination the DSNP must provide.
For the Commonwealth of Virginia, Item 288 (Q) of the 2024 Appropriations Act requires all DSNPs to operate as Fully Integrated Dually Eligible Special Needs Plans (FIDE SNP). FIDE SNPs require the highest level of Medicare-Medicaid integration. Additionally, in a recent rule change, CMS revised the definition of FIDE SNP at 42 CFR 422.2 and changed other related requirements as well, so that beginning January 1, 2025, all FIDE SNPs must operate with exclusively aligned enrollment.
While the combination of these two rules requires that DMAS adopt exclusively aligned enrollment, surveys conducted across the nation and within Virginia demonstrate that members are significantly happier with aligned enrollment. They are happier with their health plan and find it easier to access services and to navigate their multiple benefit packages than those who have not aligned their enrollment. This success is achieved through simplifying the member’s experience through integrated materials, such as provider directories and ID cards, integrated call centers, one care coordinator that can assist members with all of their Medicare and Medicaid needs, and an integrated appeals and grievance process. This change will also allow DMAS greater insight into, and oversight of, DSNP plan operations.
How this will work
With an effective date of January 1, 2025, DMAS will move any eligible dually enrolled member (see “Who Is Impacted” above) with unaligned enrollment (enrolled with one health plan for their DSNP and a different health plan for their Medicaid managed care) to the Medicaid managed care plan that matches their DSNP choice. (The member’s Medicaid managed care enrollment is determined by their choice of DSNP, as under Medicare rules, beneficiaries must have coverage choice. Virginia Medicaid, on the other hand, requires that most members enroll in managed care.) No dual that elects to enroll in a DSNP will be allowed to have unaligned enrollment.
What this means for providers
First, please be sure to verify the individual’s eligibility and managed care enrollment before
services are provided. This is always a best practice that DMAS recommends but it will be especially important since we know some of our dual eligible members will be switching health plans on January 1, 2025.
While the goal of Medicare-Medicaid integration is to make it easier for the member to access their health benefits, there are enhancements that may make the experience for providers better as well. Two specific requirements are taking effect on January 1, 2025, which may be helpful for providers. First, the health plans will be required to integrate their member and provider call centers, and second, DMAS is streamlining the process of cross-over claiming (billing Medicaid for the balance).
The health plans will integrate all member and provider call centers across Medicare and Medicaid by ensuring all call center agents can either address a caller’s Medicare and Medicaid questions or be able to complete a warm-transfer to internal staff that can answer the caller’s questions. We hope this will cut down on providers calling one call center only to be told that they must call a different one.
Currently, when a provider bills a DSNP for the Medicare portion of the service, the DSNP will pay their portion and then instruct the provider to bill the Medicaid plan for the balance. To streamline the cross-over claiming process, starting with services provided on and after January 1, 2025, the DSNP will pay both the Medicare and Medicaid portions of an aligned member’s claim at once. This avoids the need for duplicate billing processes.
Continuity of care
For those members who move from one Medicaid plan to another on January 1, the new Medicaid plan is required to follow existing continuity of care requirements (honoring existing service authorizations, allowing members to see current providers even if that provider is out-of-network) for existing Medicaid service authorizations. These requirements can be found in Section 8.11 Administrative Transitions, and particularly Section 8.11.1, Continuity of Care Upon Enrollment, of the current Cardinal Care Managed Care Contract.
Resources
We understand that as their provider you may get questions from your patients/members about this change. We hope that this bulletin will assist you in answering any question you receive but we have also included additional resources you can refer to, and refer your patient/member to, in this portion of the memo.
If you or the member has questions, the first place to call is their health plan. Below is a table with the health plan contact information.
Health Plan Name | Medicaid Plan Information | D-SNP Information |
|---|---|---|
Aetna Better Health of Virginia | https://www.aetnabetterhealth.com/virginia/index.html 1-800-279-1878 (TTY: 711) | https://www.aetnabetterhealth.com/virginia-hmosnp/ 1-855-463-0933 (TTY: 711) |
Anthem HealthKeepers | https://mss.anthem.com/va/virginia-home.html 1-800-901-0020 (TTY: 711) | 1-855-949-3321 (TTY: 711) |
Molina Healthcare of Virginia | https://www.molinahealthcare.com/members/va/en-US/pages/home.aspx 1-800-424-4518 | https://www.molinahealthcare.com/members/va/en-us/hp/medicare/medicare.aspx 1-866-403-8293 (TTY: 711) |
Sentara Health | https://www.sentarahealthplans.com/members/medicaid 1-844-563-4201 | https://www.sentarahealthplans.com/plans/medicare/sentara-community-complete-hmo-d-snp 1-855-434-3267 (TTY: 711) |
UnitedHealthCare | https://www.uhc.com/communityplan/virginia 1-855-326-9418 | 1-844-589-0514 (TTY: 711) |
You and/or your members call also find more information about exclusively aligned enrollment in the DMAS FAQ here. You can also contact DMAS by emailing us at mailto:dsnp@dmas.virginia.gov.
If members have questions about if their providers participate with their new Medicaid plan they can contact their new Medicaid plan (see above) or they also contact the Virginia Medicaid Helpline at this link or by phone at 1-800-643-2273 (TTY: 1-800-817-6608).
If members have questions about their Medicare enrollment options, they can contact their health plan or they can also contact the Virginia Insurance Counseling and Assistance Program, or VICAP, at 1-800-552-3402 (TTY 1-800-552-3402). VICAP provides free, confidential insurance counseling and information for Medicare enrollees.
To avoid disruption to claims payment through FFS and the MCOs providers must periodically check the DMAS provider portal, also known as the Provider Services Solution (PRSS), to ensure that the provider's enrollment, contact information, and license information is up to date, for all of the provider's respective service locations. Under federal rules, MCOs and DMAS are prohibited from paying claims to network providers who are not enrolled in PRSS. Additional information is provided on the MCO Provider Network Resources webpage and includes links to resources, tutorials and contact information to reach Gainwell with any provider enrollment or revalidation related questions. Dental providers should continue to enroll directly through the DMAS Dental Benefits Administrator, DentaQuest.
Virginia Medicaid Web Portal Automated Response System (ARS) Member eligibility, claims status, payment status, service limits, service authorization status, and remittance advice. | |
Medicall (Audio Response System) Member eligibility, claims status, payment status, service limits, service authorization status, and remittance advice. | 1-800-884-9730 or 1-800-772-9996 |
Provider Appeals DMAS launched an appeals portal in 2021. You can use this portal to file appeals and track the status of your appeals. Visit the website listed for appeal resources and to register for the portal. | |
Managed Care Programs Cardinal Care Managed Care and Program of All-Inclusive Care for the Elderly (PACE). In order to be reimbursed for services provided to a managed care enrolled individual, providers must follow their respective contract with the managed care plan/PACE provider. The managed care plan may utilize different guidelines than those described for Medicaid fee-for-service individuals. | |
Cardinal Care Managed Care | https://www.dmas.virginia.gov/for-providers/managed-care/cardinal-care-… |
PACE | |
Acentra Health Behavioral Health Services
| |
Provider Enrollment | In-State: 804-270-5105 Out of State Toll Free: 888-829-5373 Email: VAMedicaidProviderEnrollment@gainwelltechnologies.com |
Provider HELPLINE Monday–Friday 8:00 a.m.-5:00 p.m. For provider use only, have Medicaid Provider ID Number available. | 1-804-786-6273 1-800-552-8627 |
Aetna Better Health of Virginia | https://www.aetnabetterhealth.com/virginia/providers/index.html 1-800-279-1878
|
Anthem HealthKeepers Plus | 1-800-901-0020
|
Molina Complete Care
| 1-800-424-4524 https://www.molinahealthcare.com/providers/va/medicaid/home.aspx
|
Sentara Community Plan | 1-800-881-2166 https://www.sentarahealthplans.com/providers
|
United Healthcare | 1-844-284-0149
|
Dental Provider DentaQuest | 1-888-912-3456 |
Fee-for-Service (POS) Prime Therapeutics
| https://www.virginiamedicaidpharmacyservices.com/ 1-800-424-4046 |
Acentra Health Behavioral Health and Medical Service Authorizations | https://vamedicaid.dmas.virginia.gov/sa 1-804-622-8900 |
