Interoperability and Prior Authorization Final Rule Implementation Update
 Download PDF
Download PDF
DMAS and its Prior Authorization Contractors and Managed Care Organizations (MCOs) are implementing changes mandated by the Centers for Medicare & Medicaid Services (CMS) Interoperability and Prior Authorization Final Rule (CMS-0057-F). The purpose of this bulletin is to update providers on the implementation of the new federal Prior Authorization rules impacting existing service authorization processes. The new rule primarily shortens standard service authorization decision timeframes down from 14 days to 7 calendar days and the rules now apply to both Managed Care and Medicaid and CHIP Fee-for-Service (FFS). No action is needed from Providers. More information will be provided about the future implementation of the interoperability provisions of this final rule and the implementation of certain Application Programming Interfaces (APIs) will be communicated via a Provider Bulletin at a later date.
In accordance with 42 CFR §440.230 and §438.210, FFS service authorization contractors and Cardinal Care MCOs must adhere to these rules which include faster turnaround times for service authorization requests. Impacted FFS service authorization contractors include the Department of Behavioral Health and Developmental Services (DBHDS) for Developmental Disability (DD) Waiver Services, Modivcare for Transportation Services, Dentaquest for Dental Services, and Acentra Health for Medicaid and CHIP FFS requests.
Standard (non-urgent) requests: Response required within 7 calendar days.
Expedited (urgent) requests: Response required within 72 hours.
Decision details: Must provide a specific reason for denying a service authorization request.
Public reporting: DMAS and its MCOs must publicly report on an annual basis, certain service authorization metrics about their processes, with the first report due by March 31, 2026.
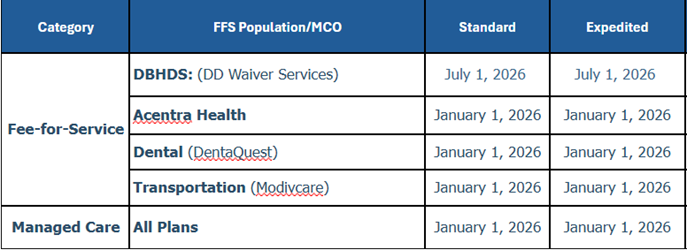
The table below illustrates expected readiness and DMAS has notified CMS[1] that we expect compliance with the new Service Authorization Decision Timeframes by the January 1, 2026 deadline with a minor exception of the service authorizations for Developmental Disability (DD) Waiver services within our Fee For Service Program. Individuals receiving DD Waiver Services can expect their non-waiver and medical service authorization decisions will meet the new timeframes on January 1, 2026, however, service authorization decisions for DD Waiver Services will meet the new timeframe requirements by July 1, 2026.
The requirement does not apply to requests to cover a drug. Timelines to respond to service authorization requests for drugs will continue to be addressed in accordance with existing contracts and policies.
Readiness Timeline Table 1.
Providers are not required to change their service authorization processes and must still comply with submission requirements found in the Service Authorization Appendices of DMAS Provider Manuals. Manuals can be found here https://vamedicaid.dmas.virginia.gov/manuals/provider-manuals-library#gsc.tab=0. It is the provider's responsibility to obtain service authorization within the required timeframes before billing DMAS. If a provider is late submitting a request, the decisions shall be based on the date it was received. The days/units that are not submitted timely are denied, and appeal rights provided.
Standard requests
Beginning January 1, 2026, standard requests must be processed within 7 calendar days after receipt of the request. In some cases, this standard request timeframe can be extended by up to 14 calendar days if:
Member or provider requests an extension (for example, to gather additional information), or
The extension is justified in the Member’s interest due to the need for the service authorization contractor or MCO to request additional medical evidence or due to extraordinary or other non-routine circumstances and is in the Member’s best interest.
[1] To date, CMS approval of our expected readiness is still pending.
Expedited requests
Beginning January 1, 2026, upon determination that the standard timeframe could seriously jeopardize the member’s life, physical or mental health, or ability to attain, maintain, or regain maximum function, the service authorization contractor or MCO must make an expedited authorization decision within 72 hours after receipt of the request. This expedited request timeframe can be extended by up to 14 calendar days for managed care service authorization requests, only if the extension is in the Member’s best interest due to the need for additional information.
Decision details
DMAS confirms that current denial decision letters from the MCOs and service authorization contractors already adhere to 42 CFR §438.242(b)(8) and 42 CFR §431.80(a) by clearly stating the reason for denial and informing Members of their right to appeal the decision.
Public reporting
To promote transparency, DMAS and its MCOs must publicly report on an annual basis, certain FFS and Managed Care service authorization metrics about their processes, beginning March 31, 2026. This initial report is required to include metrics data from calendar year 2025. Each health plan will report their metrics data annually on their websites and DMAS will report Fee-For-Service (FFS) metrics data annually on its website. The public, including providers will be able to review the FFS and Managed Care websites to gain more insight into the service authorization processes. Currently, quarterly data resources for MCO Service Authorization Performance can be found on the DMAS Dashboard [Click here]. The full list of new metrics in accordance with 42 CFR §440.230 and §438.210 is below.
A list of all items and services that require prior authorization (excluding drugs).
The percentage of standard prior authorization requests that were approved, aggregated for all items and services.
The percentage of standard prior authorization requests that were denied, aggregated for all items and services.
The percentage of standard prior authorization requests that were approved after appeal, aggregated for all items and services.
The percentage of prior authorization requests for which the timeframe for review was extended and the request was approved, aggregated for all items and services.
The percentage of expedited prior authorization requests that were approved, aggregated for all items and services.
The percentage of expedited prior authorization requests that were denied, aggregated for all items and services.
The average and median time that elapsed between the submission of a request and a determination by the payer, plan, or issuer for standard prior authorizations, aggregated for all items and services.
The average and median time that elapsed between the submission of a request and a decision by the payer, plan, or issuer, for expedited prior authorizations, aggregated for all items and services.
For Questions, please refer to the contact information below.

To avoid disruption to claims payment through FFS and the MCOs providers must periodically check the DMAS provider portal, also known as the Provider Services Solution (PRSS), to ensure that the provider's enrollment, contact information, and license information is up to date, for all of the provider's respective service locations. Under federal rules, MCOs and DMAS are prohibited from paying claims to network providers who are not enrolled in PRSS. Additional information is provided on the MCO Provider Network Resources webpage and includes links to resources, tutorials and contact information to reach Gainwell with any provider enrollment or revalidation related questions. Dental providers should continue to enroll directly through the DMAS Dental Benefits Administrator, DentaQuest.
Virginia Medicaid Web Portal Automated Response System (ARS) Member eligibility, claims status, payment status, service limits, service authorization status, and remittance advice. | |
Medicall (Audio Response System) Member eligibility, claims status, payment status, service limits, service authorization status, and remittance advice. | 1-800-884-9730 or 1-800-772-9996 |
Provider Appeals DMAS launched an appeals portal in 2021. You can use this portal to file appeals and track the status of your appeals. Visit the website listed for appeal resources and to register for the portal. | |
Managed Care Programs Cardinal Care Managed Care and Program of All-Inclusive Care for the Elderly (PACE). In order to be reimbursed for services provided to a managed care enrolled individual, providers must follow their respective contract with the managed care plan/PACE provider. The managed care plan may utilize different guidelines than those described for Medicaid fee-for-service individuals. | |
Cardinal Care Managed Care | https://www.dmas.virginia.gov/for-providers/managed-care/cardinal-care-… |
PACE | |
Provider Enrollment | In-State: 804-270-5105 Out of State Toll Free: 888-829-5373 Email: VAMedicaidProviderEnrollment@gainwelltechnologies.com |
Provider HELPLINE Monday–Friday 8:00 a.m.-5:00 p.m. For provider use only, have Medicaid Provider ID Number available. | 1-804-786-6273 1-800-552-8627 |
Aetna Better Health of Virginia | https://www.aetnabetterhealth.com/virginia/providers/index.html 1-800-279-1878
|
Anthem HealthKeepers Plus | 1-800-901-0020
|
Humana Healthy Horizons Provider Services Call Center | 1-844-881-4482 (TTY: 711) |
Sentara Community Plan | 1-800-881-2166 https://www.sentarahealthplans.com/providers
|
United Healthcare | 1-844-284-0146
|
Acentra Health Behavioral Health and Medical Service Authorizations | https://vamedicaid.dmas.virginia.gov/sa 1-804-622-8900 |
Dental Provider DentaQuest | 1-888-912-3456 |
Fee-for-Service (POS) Prime Therapeutics
| https://www.virginiamedicaidpharmacyservices.com/ 1-800-932-6648 |
