Drug Utilization Review (DUR) Meeting, Pharmacy and Therapeutics (P&T) Meeting, and Prescription Monitoring Program (PMP) Compliance Effective July 1, 2025
 Download PDF
Download PDF
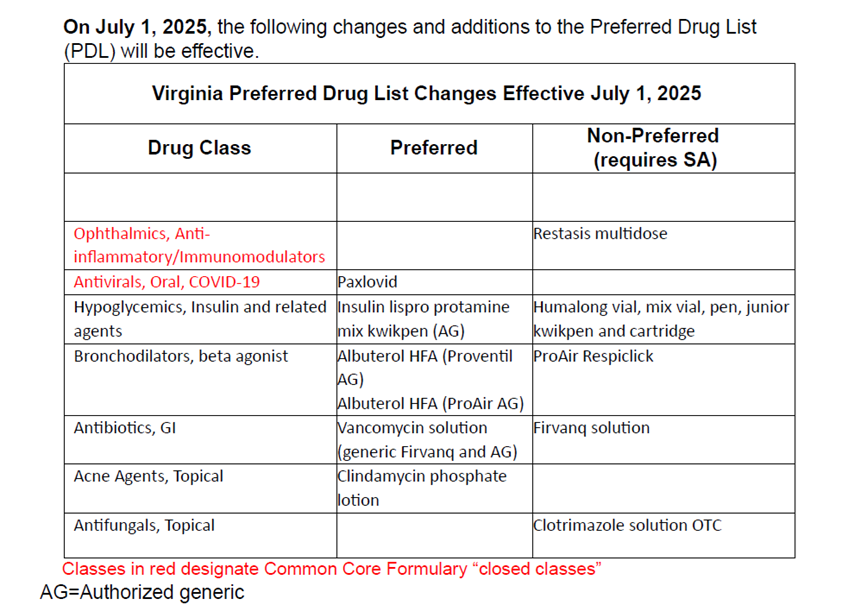
The purpose of this bulletin is to notify providers about routine changes to new drug service authorization (SA) requirements for drugs reviewed clinically and through fiscal analysis by the Drug Utilization Review (DUR) Board in March 2025 and to the Virginia Medicaid Fee-for-Service Preferred Drug List (PDL) program (also known as the Common Core Formulary, or CCF) for drugs reviewed by the Department’s Pharmacy and Therapeutics Committee in April 2025. Additionally, this bulletin will provide an overview of a survey completed by DMAS in April 2025 to assess compliance of Medicaid providers in checking the PMP when prescribing controlled substances.
The Drug Utilization Review Board is authorized by 12VAC30-130-340 and the Pharmacy and Therapeutics Committee is authorized by 12VAC30-130-1000. The meetings of these committees are open to the public and are posted on the Virginia Town Hall meetings page.
The PDL/CCF is a list of preferred drugs, by select therapeutic class, for which the Medicaid Fee-for-Service (FFS) program may allow payment without requiring a SA. The PDL/CCF program aims to provide clinically effective and safe drugs for its members in a cost-effective manner. Your continued compliance with and support of this program and its policies are critical to its success.
The PDL/CCF is applicable to the Medicaid and FAMIS Plus FFS populations, and non-dual eligible members covered under the Managed Care Program. The Virginia Medicaid PDL/CCF does not apply to members enrolled in FAMIS or Members with Medicare Part D Plans.
As part of the annual DUR survey submitted to the Centers for Medicare and Medicaid Services (CMS), DMAS must report the percentage of providers that check the PMP before prescribing controlled substances. This information was collected using a survey that was sent to all enrolled providers with prescribing authority in April 2025. The requirements for providers to check the PMP are outlined in https://law.lis.virginia.gov/vacode/title54.1/chapter25.2/
March 2025 DUR Board Summary
The DUR Board reviewed 11 new medications - Aqneursa™, Danziten™, Itovebi™, Lazcluze™, Lodoco®, Miplyffa™, Voranigo®, Vyalev™, Xdemvy™, Xolremdi® and Yorvipath®. The Board reviewed and approved service authorization criteria for these medications.
The DUR Board reviewed and approved updates to the service authorization criteria for Rezdiffra™.
The DUR Board reviewed three pipeline drugs: avutometinib + defactinib oral, clesrovimab IM and sepiapterin oral.
The Board reviewed the results of several utilization analyses:
the impact reports for 11 new DUR medications (Aqneursa™, Danziten™, Itovebi™, Lazcluze™, Lodoco®, Miplyffa™, Voranigo®, Vyalev™, Xdemvy™, Xolremdi® and Yorvipath®);
current use of opioids and benzodiazepines;
concurrent use of opioids and antipsychotics;
overlaps in opioids, benzodiazepines, and antipsychotics;
naloxone and buprenorphine utilization for members on opioids;
antipsychotic medications in children;
antidepressant medications in children;
mood stabilizer medications in children;
overlaps in antipsychotics,
antidepressants and mood stabilizers in children;
ProDUR reports; RetroDUR reports and utilization analysis reports.
April 2025 P&T Meeting PDL/CCF Changes
April 2025 PMP Survey Results
Response rate to survey | 3% |
Percentage of prescribers who reported they do not prescribe controlled substances | 47.7% |
Percentage of prescribers who reported they do prescribe controlled substances | 52.3% |
Percentage of prescribers who check the PMP before prescribing controlled substances | 86.6% |
To avoid disruption to claims payment through FFS and the MCOs providers must periodically check the DMAS provider portal, also known as the Provider Services Solution (PRSS), to ensure that the provider's enrollment, contact information, and license information is up to date, for all of the provider's respective service locations. Under federal rules, MCOs and DMAS are prohibited from paying claims to network providers who are not enrolled in PRSS. Additional information is provided on the MCO Provider Network Resources webpage and includes links to resources, tutorials and contact information to reach Gainwell with any provider enrollment or revalidation related questions. Dental providers should continue to enroll directly through the DMAS Dental Benefits Administrator, DentaQuest.
Virginia Medicaid Web Portal Automated Response System (ARS) Member eligibility, claims status, payment status, service limits, service authorization status, and remittance advice. | |
Medicall (Audio Response System) Member eligibility, claims status, payment status, service limits, service authorization status, and remittance advice. | 1-800-884-9730 or 1-800-772-9996 |
Provider Appeals DMAS launched an appeals portal in 2021. You can use this portal to file appeals and track the status of your appeals. Visit the website listed for appeal resources and to register for the portal. | |
Managed Care Programs Cardinal Care Managed Care and Program of All-Inclusive Care for the Elderly (PACE). In order to be reimbursed for services provided to a managed care enrolled individual, providers must follow their respective contract with the managed care plan/PACE provider. The managed care plan may utilize different guidelines than those described for Medicaid fee-for-service individuals. | |
Cardinal Care Managed Care | https://www.dmas.virginia.gov/for-providers/managed-care/cardinal-care-… |
PACE | |
Provider Enrollment | In-State: 804-270-5105 Out of State Toll Free: 888-829-5373 Email: VAMedicaidProviderEnrollment@gainwelltechnologies.com |
Provider HELPLINE Monday–Friday 8:00 a.m.-5:00 p.m. For provider use only, have Medicaid Provider ID Number available. | 1-804-786-6273 1-800-552-8627 |
Aetna Better Health of Virginia | https://www.aetnabetterhealth.com/virginia/providers/index.html 1-800-279-1878
|
Anthem HealthKeepers Plus | 1-800-901-0020
|
Humana Healthy Horizons Provider Services Call Center | 1-844-881-4482 (TTY: 711) |
Molina Complete Care
| 1-800-424-4518 https://www.molinahealthcare.com/providers/va/medicaid/home.aspx
|
Sentara Community Plan | 1-800-881-2166 https://www.sentarahealthplans.com/providers
|
United Healthcare | 1-844-284-0149
|
Acentra Health Behavioral Health and Medical Service Authorizations | https://vamedicaid.dmas.virginia.gov/sa 1-804-622-8900 |
Dental Provider DentaQuest | 1-888-912-3456 |
Fee-for-Service (POS) Prime Therapeutics
| https://www.virginiamedicaidpharmacyservices.com/ 1-800-932-6648 |
