Deemed Newborns Automated Process
 Download PDF
Download PDF
The purpose of this bulletin is to alert providers that, effective Monday, August 28, 2023, Department of the Medical Assistance Services (DMAS) is implementing a new automated method for enrolling deemed newborns.
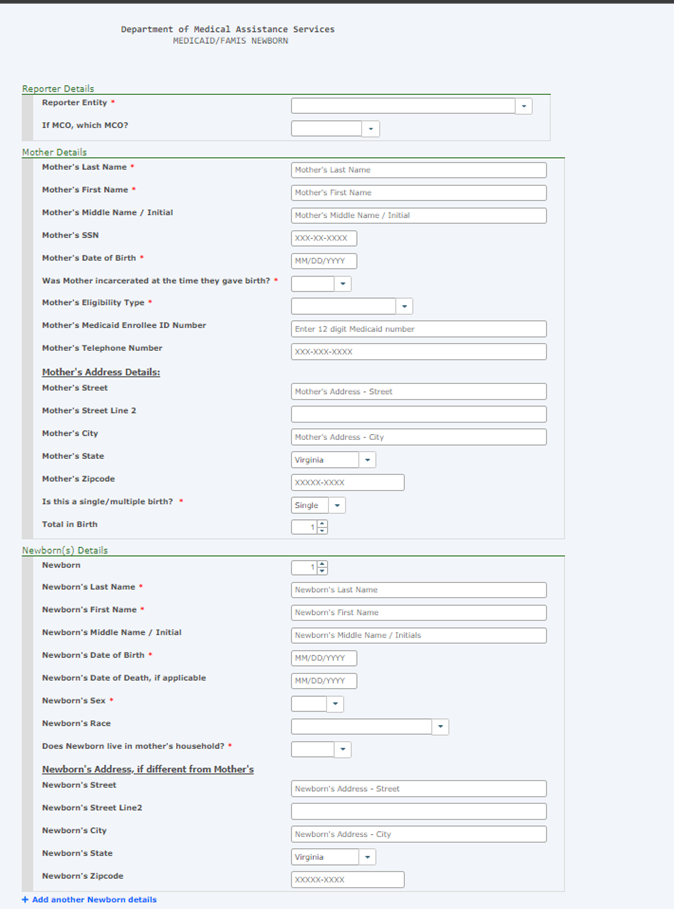
Our systems will be enhanced to receive newborns reported through the Medicaid Enrollment System (MES) and auto enroll them into the Virginia Case Management System (VaCMS). Minimal changes have been made to the E-213 enrollment form (as shown below). Coverage for eligible deemed newborns will continue to be effective on their date of birth.
This process will increase efficiency allowing timely access to benefits. In the event of an unsuccessful transmission, the DMAS Newborn and Member Enrollment (NAME) unit will review and process those newborns manually. Reasons for unsuccessful transmission include:
- If the mother has no active or pending Medicaid coverage at the time of the child's birth.
- If the mother is deceased.
- If the mother’s eligibility is pending, then the child’s eligibility cannot be fully determined.
- Newborns with aliases of Baby Boy and Baby Girl.
- Newborns with a non-Virginia address.
Inquiries can be made via the following mailbox after 30 days of submitting the E-213 enrollment form: newborn-providers@dmas.virginia.gov.
PROVIDER CONTACT INFORMATION & RESOURCES | |
Virginia Medicaid Web Portal Automated Response System (ARS) Member eligibility, claims status, payment status, service limits, service authorization status, and remittance advice. | |
Medicall (Audio Response System) Member eligibility, claims status, payment status, service limits, service authorization status, and remittance advice. | 1-800-884-9730 or 1-800-772-9996 |
Acentra Health Service authorization information for fee-for-service members.
| |
Provider Appeals DMAS launched an appeals portal in 2021. You can use this portal to file appeals and track the status of your appeals. Visit the website listed for appeal resources and to register for the portal. | |
Managed Care Programs Medallion 4.0, Commonwealth Coordinated Care Plus (CCC Plus), and Program of All-Inclusive Care for the Elderly (PACE). In order to be reimbursed for services provided to a managed care enrolled individual, providers must follow their respective contract with the managed care plan/PACE provider. The managed care plan may utilize different guidelines than those described for Medicaid fee-for-service individuals. | |
Medallion 4.0 | |
CCC Plus | |
PACE | |
Magellan Behavioral Health Behavioral Health Services Administrator, check eligibility, claim status, service limits, and service authorizations for fee-for-service members. | www.MagellanHealth.com/Provider www.magellanofvirginia.com, email: VAProviderQuestions@MagellanHealth.com,or Call: 1-800-424-4046 |
Provider Enrollment | In-State: 804-270-5105 Out of State Toll Free: 888-829-5373 Email: VAMedicaidProviderEnrollment@gainwelltechnologies.com |
Provider HELPLINE Monday–Friday 8:00 a.m.-5:00 p.m. For provider use only, have Medicaid Provider ID Number available. | 1-804-786-6273 1-800-552-8627 |
Aetna Better Health of Virginia | www.aetnabetterhealth.com/Virginia 1-855-270-2365 1-866-386-7882 (CCC+) |
Anthem HealthKeepers Plus | www.anthem.com/vamedicaid 1-833-207-3120 1-833-235-2027 (CCC+) |
Molina Complete Care
| 1-800-424-4524 (CCC+) 1-800-424-4518 (M4) |
Optima Family Care | 1-800-643-2273 1-844-374-9159 (CCC+) |
United Healthcare | 1-844-284-0149 1-855-873-3493 (CCC+) |
Dental Provider DentaQuest | 1-888-912-3456 |
