Information on the Eligibility Renewal Process - REVISED
 Download PDF
Download PDF
This bulletin (which supersedes the bulletin entitled “Information on the Eligibility Renewal Process” dated March 24, 2023) is a REVISION to the previous bulletin. The purpose of this bulletin is to provide information about the eligibility renewal process over the next 12 months, including how Medicaid and FAMIS members can determine when their renewals will occur.
Renewal dates are grouped according to the date of the member’s last renewal, as shown in the chart below.
|
|
Renewal Process Start |
||
|
May 2023 |
March 2023 |
||
|
March – October 2020 |
& |
June 2023 |
April 2023 |
|
November 2020 – March 2021 |
& |
July 2023 |
May 2023 |
|
April – September 2021 |
& |
August 2023 |
June 2023 |
|
October 2021 |
& |
September 2023 |
July 2023 |
|
November 2021 |
& |
October 2023 |
August 2023 |
|
December 2021 |
& |
November 2023 |
September 2023 |
|
January – February 2022 |
& |
December 2023 |
October 2023 |
|
March – May 2022 |
& |
January 2024 |
November 2023 |
|
June – October 2022 |
& |
February 2024 |
December 2023 |
|
November 2022 – February 2023 |
& |
March 2024 |
January 2024 |
|
March – April 2023 |
& |
April 2024 |
February 2024 |
If a member does not know their renewal date, they can call their local Department of Social Services (go to the following link to identify that office: https://www.dss.virginia.gov/localagency/index.cgi), or Cover Virginia (1-855-242-8282) (TTY: 1-888-221-1590).
The following functionality will be available on Saturday, April 1, 2023:
If a provider would like to determine the renewal date for a Medicaid member that they are serving, they can go to the Member Eligibility Inquiry page in the Provider Services Solution (PRSS) system. The response will show the member’s renewal date as demonstrated by the red box below. Once the provider has the “case review date” the provider should review the chart above to determine when the renewal will occur.
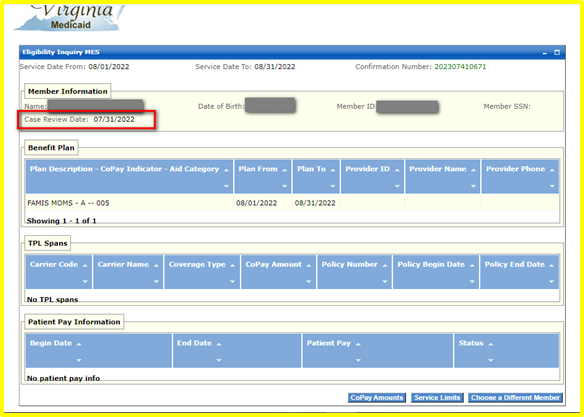
If providers have any difficulties accessing this screen, they are encouraged to visit the Helpful Links tab in PRSS and review the Provider Reference Material, especially the User Guide, Frequently Asked Questions (FAQ), and Computer Based Training (CBT).
Starting now, some Medicaid and FAMIS members will receive a letter in the mail informing them that their renewal was completed. If DMAS needs more information to complete the renewal, the member will receive a packet in the mail with options for submitting the renewal online, via phone, or by completing the documentation and returning it in person or by mail/fax.
For more details about the return to regular renewal operations, providers are encouraged to access the following resources on the Cover Virginia Website: Renewal Process Flowchart, Renewal Process Flow Sheet: Step-By-Step, Renewal Process Flow Sheet: Where Are You?, and Toolkits and Materials.
For questions, additional help, or language assistance services or large-print, Medicaid and FAMIS members are encouraged to call Cover Virginia at 1-855-242-8282 (TTY: 1-888-221-1590) or send an email to: covervirginia@dmas.virginia.gov.\
|
PROVIDER CONTACT INFORMATION & RESOURCES |
|
|
Virginia Medicaid Web Portal Automated Response System (ARS) Member eligibility, claims status, payment status, service limits, service authorization status, and remittance advice. |
|
|
Medicall (Audio Response System) Member eligibility, claims status, payment status, service limits, service authorization status, and remittance advice. |
1-800-884-9730 or 1-800-772-9996 |
|
KEPRO Service authorization information for fee-for-service members. |
|
|
Provider Appeals DMAS launched an appeals portal in 2021. You can use this portal to file appeals and track the status of your appeals. Visit the website listed for appeal resources and to register for the portal. |
|
|
Managed Care Programs Medallion 4.0, Commonwealth Coordinated Care Plus (CCC Plus), and Program of All-Inclusive Care for the Elderly (PACE). In order to be reimbursed for services provided to a managed care enrolled individual, providers must follow their respective contract with the managed care plan/PACE provider. The managed care plan may utilize different guidelines than those described for Medicaid fee-for-service individuals. |
|
|
Medallion 4.0 |
|
|
CCC Plus |
|
|
PACE |
|
|
Magellan Behavioral Health Behavioral Health Services Administrator, check eligibility, claim status, service limits, and service authorizations for fee-for-service members. |
www.MagellanHealth.com/Provider For credentialing and behavioral health service information, visit: www.magellanofvirginia.com, email: VAProviderQuestions@MagellanHealth.com,or Call: 1-800-424-4046 |
|
Provider HELPLINE Monday–Friday 8:00 a.m.-5:00 p.m. For provider use only, have Medicaid Provider ID Number available. |
1-804-786-6273 1-800-552-8627 |
|
Aetna Better Health of Virginia |
www.aetnabetterhealth.com/Virginia 1-855-270-2365 1-866-386-7882 (CCC+) |
|
Anthem HealthKeepers Plus |
1-833-207-3120 1-833-235-2027 (CCC+) |
|
Molina Complete Care |
1-800-424-4524 (CCC+) 1-800-424-4518 (M4) |
|
Optima Family Care |
1-800-643-2273 1-844-374-9159 (CCC+) |
|
United Healthcare |
1-844-284-0149 1-855-873-3493 (CCC+) |
|
Virginia Premier |
1-800-727-7536 (TTY: 711), www.virginiapremier.com |
