Coverage of Single-Dose COVID-19 Vaccine Administration
 Download PDF
Download PDF
The purpose of this memorandum is to inform providers:
- That the Virginia Department of Medical Assistance Services (DMAS) fee-for-service (FFS) and all contracted managed care plans will cover one (1) new COVID-19 vaccine product and one (1) new COVID-19 vaccine administration code for all full benefit Medicaid and FAMIS populations
- Of pharmacy procedures for the new COVID-19 vaccine product and administration
Further contact information is included at the bottom of this document.
The codes below will be covered by DMAS FFS and all DMAS Managed Care Organizations (MCOs) pending the issuance of an Emergency Use Authorization (EUA) by the Food and Drug Administration (FDA). The effective date of service will be the date of issuance of an EUA, and no earlier than February 26, 2021.
|
CPT code |
Description |
Reimbursement rate |
|
91303 |
SARSCOV2 VAC AD26 .5ML Janssen Covid-19 Vaccine |
$0.01 |
|
0031A |
ADM SARSCOV2 VAC AD26 .5ML Janssen Covid-19 Vaccine Admin. |
$28.39 |
The Centers for Medicare and Medicaid Services (CMS) anticipates that, at this time, providers will not incur a cost for vaccine products (CPT 91303). Providers should not bill for a vaccine product if they received it for free.
For questions on coverage for members enrolled in a managed care organization, refer to the contact information listed at the end of this document.
Pharmacy procedure for COVID-19 vaccine
Please refer to the Medicaid Memo “Pharmacy Procedure For COVID-19 Vaccine” for further information on pharmacy procedures for COVID-19 vaccine products and administration. Note that for single dose vaccines, submission clarification codes are not required.
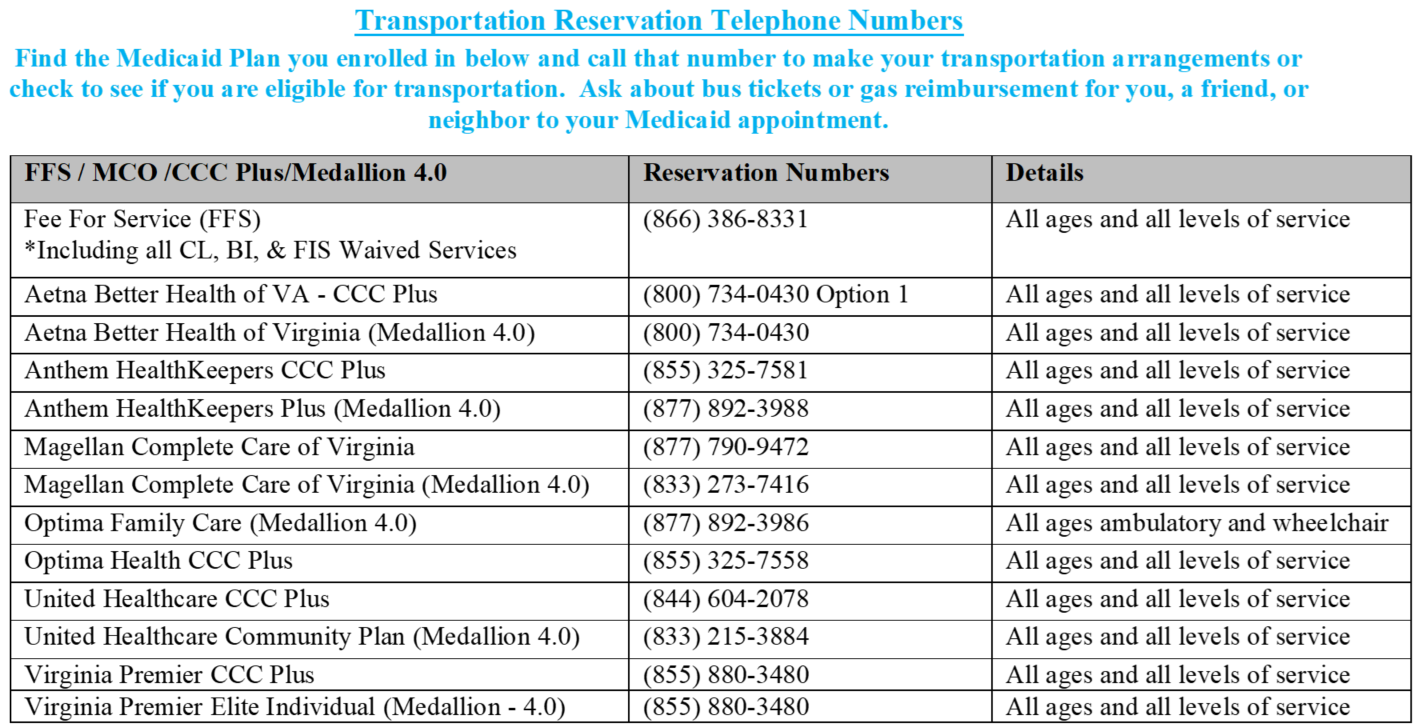
Members (or providers on behalf of members) who require transportation assistance for their vaccinations, can schedule transportation by calling the appropriate number on this contact list:
*************************************************************************************
|
PROVIDER CONTACT INFORMATION & RESOURCES |
|
|
Virginia Medicaid Web Portal Automated Response System (ARS) Member eligibility, claims status, payment status, service limits, service authorization status, and remittance advice. |
|
|
Medicall (Audio Response System) Member eligibility, claims status, payment status, service limits, service authorization status, and remittance advice. |
Call: 1-800-884-9730, or 1-800-772-9996 |
|
KEPRO Service authorization information for fee-for-service members. |
Visit: https://dmas.kepro.com/
|
|
Managed Care Programs Medallion 4.0, Commonwealth Coordinated Care Plus (CCC Plus), and Program of All-Inclusive Care for the Elderly (PACE). In order to be reimbursed for services provided to a managed care enrolled individual, providers must follow their respective contract with the managed care plan/PACE provider. The managed care plan may utilize different guidelines than those described for Medicaid fee-for-service individuals. |
|
|
Medallion 4.0 |
|
|
CCC Plus |
|
|
PACE |
|
|
Magellan Behavioral Health Behavioral Health Services Administrator, check eligibility, claim status, service limits, and service authorizations for fee-for-service members. |
Visit: http://www.magellanhealth.com/Provider For credentialing and behavioral health service information: Visit: www.magellanofvirginia.com Email: VAProviderQuestions@MagellanHealth.com Call: 1-800-424-4046
|
|
Provider HELPLINE Monday–Friday 8:00 a.m.-5:00 p.m. For provider use only, have Medicaid Provider ID Number available. |
Call: 1-804-786-6273, or 1-800-552-8627 |
|
Aetna Better Health of Virginia |
Visit: www.aetnabetterhealth.com/virginia Call: 1-800-279-1878 |
|
Anthem HealthKeepers Plus |
Visit: www.anthem.com/vamedicaid, or Call: 1-800-901-0020 |
|
Magellan Complete Care of Virginia |
Visit: www.MCCofVA.com Call: 1-800-424-4518 (TTY 711), or 1-800-643-2273 |
|
Optima Family Care |
Call: 1-800-881-2166 |
|
United Healthcare |
Visit: www.uhccommunityplan.com/VA, or Call: 1-844-752-9434, TTY 711 |
|
Virginia Premier |
Call: 1-800-727-7536 (TTY: 711) |
